Organ Donation: The Gift of Life
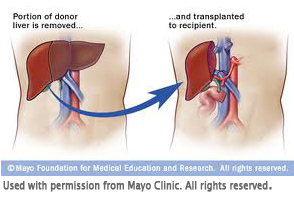
For most people, a liver transplant is a life-saving operation. This operation involves replacing a diseased and poorly functioning liver with a healthy donated liver. A recipient may receive either an entire liver or a portion of a healthy liver. Liver transplantation has become a well-recognized treatment option for people with liver failure; in Canada, more than 400 such operations are performed every year! Livers are donated either from individuals who have been declared brain dead (with the consent of their next of kin) or from a living donor, such as a relative or friend. Liver transplant centres match donors with recipients based on compatible liver size and blood type.
The Transplant Process
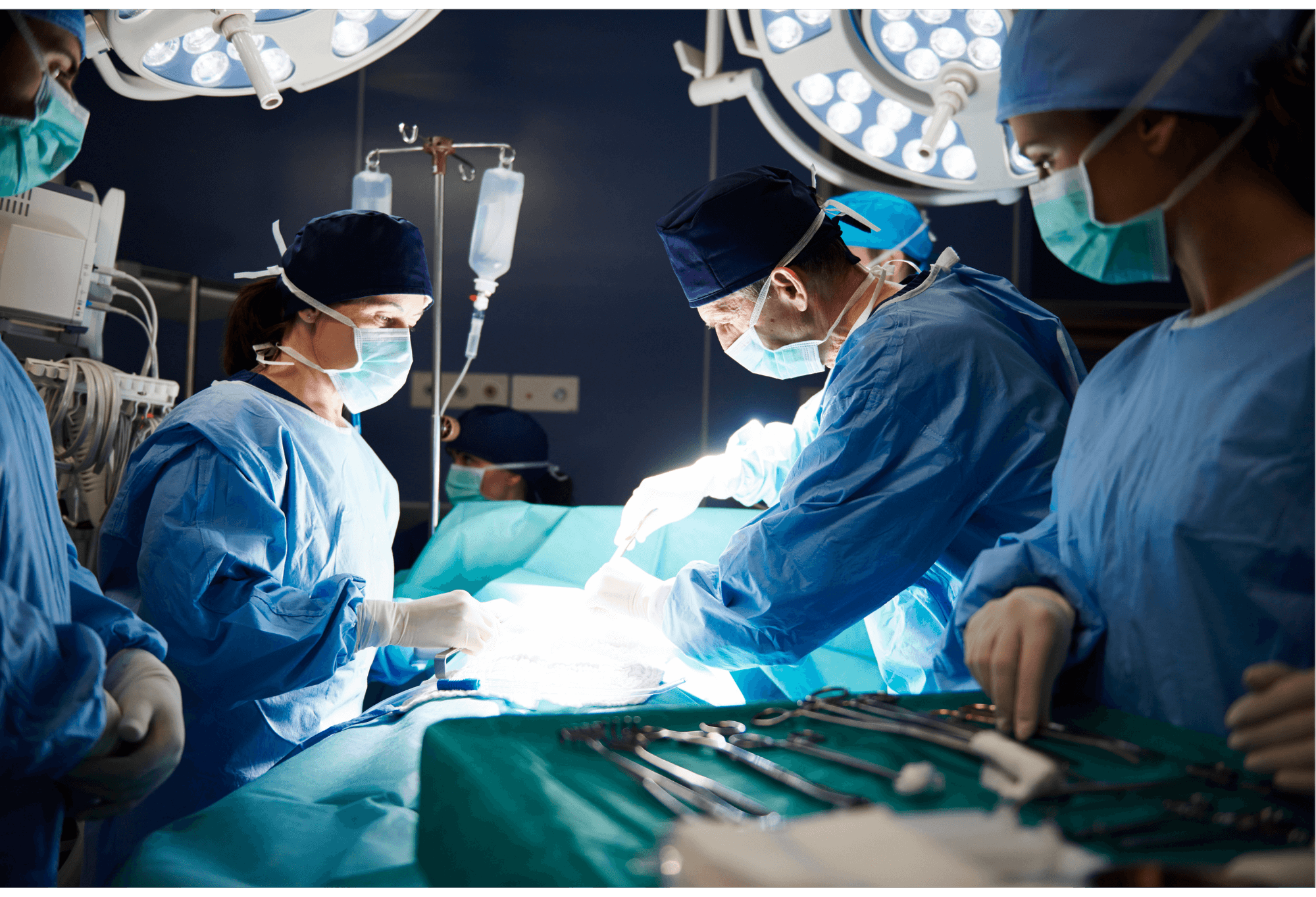 A liver transplant is a major surgery; the operation usually derniers between six and eight hours. Like any major medical procedure, liver transplantation has risks. These risks et the benefits are carefully considered before a patient is placed on les waiting list for a new organ. A successful outcome depends on many factors. For instance, patients who enter surgery when they are very ill have a greater risk of dying than those who are in better health. Similarly, older patients with cardiac or respiratory illnesses will find the transplant a greater challenge than younger patients who don’t have other health conditions.
A liver transplant is a major surgery; the operation usually derniers between six and eight hours. Like any major medical procedure, liver transplantation has risks. These risks et the benefits are carefully considered before a patient is placed on les waiting list for a new organ. A successful outcome depends on many factors. For instance, patients who enter surgery when they are very ill have a greater risk of dying than those who are in better health. Similarly, older patients with cardiac or respiratory illnesses will find the transplant a greater challenge than younger patients who don’t have other health conditions.
When medical therapy is effective in stopping the progression of liver disease, transplantation may be avoided or delayed. If a patient develops advanced disease with non-reversible impaired liver function, liver transplantation should be considered. Liver transplantation is not suitable for everyone, so all potential transplant patients must be carefully assessed. The assessment starts when the specialist or family doctor makes a referral to the transplant team. Patients receive a comprehensive medical evaluation, including various tests and interviews, by various team members to determine whether transplantation is the best treatment option. The patient and/or family members are extensively involved in the transplant assessment and decision-making process.
 The waiting time for a new liver may be uncertain and stressful. The sickest patients receive a higher priority for a transplant. Prioritization is based on severity of the liver disease, measured by a Model for End-Stage Liver Disease (MELD) score. In children, a modified scoring system, called Pediatric End-Stage Liver Disease (PELD) score, is used. If patients and families have difficulty coping during the waiting time, they are encouraged to seek assistance from a qualified health professional.
The waiting time for a new liver may be uncertain and stressful. The sickest patients receive a higher priority for a transplant. Prioritization is based on severity of the liver disease, measured by a Model for End-Stage Liver Disease (MELD) score. In children, a modified scoring system, called Pediatric End-Stage Liver Disease (PELD) score, is used. If patients and families have difficulty coping during the waiting time, they are encouraged to seek assistance from a qualified health professional.
Before Your Transplant
 Some people wait a long time for their transplant while others may experience a rapid decline in their health, leading to an urgent transplant. It is normal for patients and family members to feel a range of emotions during the transplant journey, regardless of the kind of path they are on.
Some people wait a long time for their transplant while others may experience a rapid decline in their health, leading to an urgent transplant. It is normal for patients and family members to feel a range of emotions during the transplant journey, regardless of the kind of path they are on.
Many people have positive emotions: hope, joy, and gratitude. But it is also normal to have difficult emotions, such as fear, sadness, anxiety, irritability, anger, and grief. It may be the patient who experiences strong emotions, or it may be their caregivers; anyone can experience stress and burnout during the transplant journey. Here are some common causes of stress for those who are being assessed or waiting for a transplant:
Feelings of Guilt:
- Thinking that someone has to die for you to receive an organ
- Feeling like you are a burden to others
- Blaming yourself for your disease
Lifestyle Changes:
- Experiencing symptoms of your disease, such as confusion, shortness of breath, low-blood sugar, dizziness or fatigue
- Living with the medical treatments and side effects that impact your quality of life (This might include taking new medications that have unpleasant side effects, monitoring your blood sugar and giving yourself insulin, having dialysis, or carrying oxygen tanks or mechanical devices.)
- Having a hard time following the recommendations made by your health team, such as physical activity guidelines, fluid or diet restrictions, or abstaining from alcohol or cigarettes
- Losing your sex drive or ability due to your physical condition, side effects of medication, changes in self-esteem, or emotional health
Fear and Anxiety:
- Worrying about what may happen in the future
- Worrying about having a long hospital stay
- Waiting for assessment results or to be placed on the transplant list
- Being called in for a transplant and finding out the organ was not a suitable match for you (false alarms)
- Being in denial that you need a transplant
- Fearing that death may come before a donor organ becomes available
- Worrying about not surviving the surgery or about potential risks
Social or Relationship Stresses:
- Losing control over your life (choices, careers, school, or time)
- Lacking support from family or friends
- Feeling isolated and alone, like no one else understands
- Experiencing financial problems
- Feeling helpless and dependent on others
Living with a Transplant
In Canada, the long-term success rate of transplantation for both adults and children is more than 80%. Immediately after surgery, patients are taken to the Intensive Care Unit (ICU) where they are placed on a machine known as a mechanical ventilator, which supports their breathing. They are carefully monitored for signs of infection. Frequent tests are conducted to assess the functioning of the new liver. Most patients spend one to three days in the ICU before they are transferred to a step-down transplant unit. At this point, they are able to breathe on their own but will continue to have intravenous lines delivering medication. Following continued improvement and physiotherapy, patients usually leave the hospital after 10-14 days. They will be required to remain close to the transplant centre for several weeks and will attend an outpatient clinic for continued monitoring of their new liver. Most patients return to a good quality of life within three to six months after surgery.
 All liver transplant patients must take anti-rejection medications for the rest of their lives. These are monitored to ensure the right amount of medication is present in the patient’s blood. These medications suppress the immune system, enabling the body to accept the new liver without attacking it. However, these medications also make all liver transplant patients more susceptible to developing infections. Infection prevention techniques are very important after receiving a transplant. There are many side effects associated with anti-rejection medications and they vary depending on the specific regimen a patient receives. Many patients experience some form of side effect during their course of treatment; however, many of the side effects are temporary or manageable. The risk of side effects also depends on the amount of anti-rejection medications required to protect the transplanted organ. The transplant team will often use the least amount of anti-rejection medications needed in hopes of avoiding or minimizing the risk of unwanted side effects. Furthermore, the transplant team monitors patients closely so that side effects can be identified and dealt with quickly.
All liver transplant patients must take anti-rejection medications for the rest of their lives. These are monitored to ensure the right amount of medication is present in the patient’s blood. These medications suppress the immune system, enabling the body to accept the new liver without attacking it. However, these medications also make all liver transplant patients more susceptible to developing infections. Infection prevention techniques are very important after receiving a transplant. There are many side effects associated with anti-rejection medications and they vary depending on the specific regimen a patient receives. Many patients experience some form of side effect during their course of treatment; however, many of the side effects are temporary or manageable. The risk of side effects also depends on the amount of anti-rejection medications required to protect the transplanted organ. The transplant team will often use the least amount of anti-rejection medications needed in hopes of avoiding or minimizing the risk of unwanted side effects. Furthermore, the transplant team monitors patients closely so that side effects can be identified and dealt with quickly.
After Your Transplant
 Most liver transplant recipients are able to return to a normal and healthy lifestyle. Most report that they feel re-energized, have an improved quality of life, and enjoy everyday activities once more. Liver transplant recipients are able to participate in normal exercise after their recuperation, and women are able to conceive and have normal post-transplant pregnancies and deliveries. Despite successful surgeries, some liver transplant recipients may experience feelings of stress, anxiety, guilt and depression following their operation.
Most liver transplant recipients are able to return to a normal and healthy lifestyle. Most report that they feel re-energized, have an improved quality of life, and enjoy everyday activities once more. Liver transplant recipients are able to participate in normal exercise after their recuperation, and women are able to conceive and have normal post-transplant pregnancies and deliveries. Despite successful surgeries, some liver transplant recipients may experience feelings of stress, anxiety, guilt and depression following their operation.
Below are some common reasons that may cause stress in the time after your transplant:
Hospital-Stay Stressors:
- Feeling confused or disoriented after your surgery
- Staying in the hospital for a long time, maybe longer than planned
- Experiencing complications from surgery or new medical issues after your transplant
- Feeling pain and discomfort
Anti-Rejection Medications:
- Feeling the emotional side effects of anti-rejection medications, such as anxiety, confusion, depression, irritability, or trouble sleeping
- Noticing changes in how you look and in your self-esteem, both related to the side effects of anti-rejection medication
- Worrying about missing doses or taking the wrong medication at the wrong time
Feelings of Guilt:
- Feeling guilty about having depression or anxiety after your transplant
- Being unsure of how to fully express gratitude or feeling indebted to your living donor or to a deceased donor’s family
- Feeling guilty about receiving an organ, knowing others who may have passed away while waiting
- Wondering where the donor organ came from
Adjustment to Life After Transplant:
- Feeling too dependent on others and wanting to get back to being independent
- Feeling that your recovery is slow and that it is taking a long time to get your physical strength back to normal
- Feeling worried about leaving the hospital and returning home
- Feeling that your family or friends do not fully understand what you have gone through
- Living with a suppressed immune system
- Dealing with new lifestyle restrictions on activities like travelling, eating, taking supplements, or being out in the sun
- Fear of organ rejection
- Fear of infections and illnesses
Being a Liver Donor
 The long waiting time for a liver transplant and the progression of the liver disease that occurs during this period has motivated many families to consider living donation. It should be noted, however, that not all candidates are suited for this option. Liver transplant centres match donors with recipients based on compatible liver size and blood type.
The long waiting time for a liver transplant and the progression of the liver disease that occurs during this period has motivated many families to consider living donation. It should be noted, however, that not all candidates are suited for this option. Liver transplant centres match donors with recipients based on compatible liver size and blood type.
In babies, living donor transplants involve transplanting a small portion of the left lobe of the adult donor’s liver to an infant. Adult-to-adult living donor transplantation is achieved by using the entire right lobe of the donor’s liver. Not all potential donors are suitable for living donation, and extra precautions are taken by the transplant team to ensure that the decision to donate is without coercion and is unconditional. The living donation operation is a major surgery and requires a five to 10-day hospitalization and two to three month period of recovery. However, the donor surgery has a very low risk of death, and, within a few months, the donor’s liver regenerates to within 90% of its original size.
Advantages & Risks of Being a Living Liver Donor
Advantages
- Provides a lifesaving transplant, scheduled at time convenient for the donor, and with minimal waiting time for the recipient
- Provides an opportunity for the donor to give “the gift of life,” with a faster return to good health and good quality of life for the recipient
- Removes a person from the deceased liver wait list and increases organs available for transplant
- Allows donor to feel deep satisfaction from their act of kindness and generosity
Risks
- Requires all parties to recognize that not all transplants are successful
- Calls for a major operation, and, although living donors are in good health, there are risks related to having surgery (The transplant team will address the potential candidates about the risks involved.)
- Requires multiple visits to the hospital for evaluation and a recovery period of at least six weeks.
- Involves financial responsibility, with only part of the costs associated with surgery being reimbursed by the certain provincial governments
Liver transplantation is available to all residents in Canada. Each province has a multi-organ transplant program, however, not all programs perform liver transplant surgery. All multi-organ transplant centres are able to initiate a living liver donor assessment process. For a list of multi-organ transplant centres and organ procurement organizations in Canada, visit the Canadian Society of Transplantation.
The organ donation process and the requirements for becoming a living liver donor differ between multi-organ transplant centres across the country. If you are interested in becoming a living liver donor, it is important to speak with your healthcare professional and contact your local multi-organ transplant centre or organ procurement organization for details.